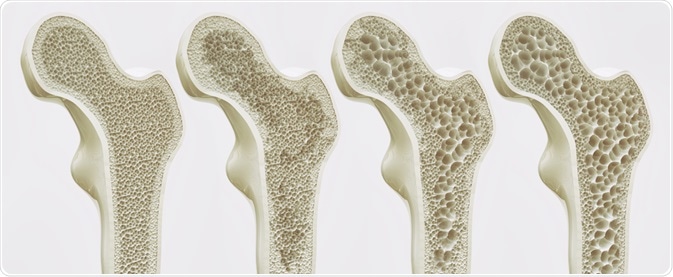
MONOTHERAPY?: Osteoporosis and Osteopenia
We have been conditioned to accept the concept of monotherapy for every disease or degenerative process. That works fine for strep throat treated with penicillin, but beyond antibiotic therapies for specific infections, most of our physical healing requires innumerable component processes and chemical synergies.
Let’s take bone density, for example. We have been led to believe that calcium is the key to fixing osteopenia and osteoporosis. The bisphosphonate drugs are ‘the answer’ we are told – again MONOTHERAPY. It started with a daily dose, then a weekly pill, then a once a month injection, and on and on, but still the same monotherapy. These drugs are not very effective and essentially only slow bone resorption, not promoting bone regeneration (osteogenesis). Look it up (Drake, et.al., Mayo Clin Proc. 2008 Sep; 83(9): 1032–1045). And in general, bone densities continue to decline; although much more slowly, and usually these drugs are recommended to be discontinued after 3-5 years of this monotherapy treatment.
The FDA recommends these medications and calcium. We are now so far ahead of these recommendations in our knowledge of DNA and biochemistry. Time for them to get up to speed. So how do we really make bone? Why don’t we just give the body what it requires so it can make its bone properly?
Osteoporosis Of The Vertebrae
The osteoblast cell is the bone maker, in contrast to the osteoclast. How, then, do we crank up this osteoblast machinery?
Here’s how it works:
The DNA in the osteoblast MUST have a molecular tweek from a heterodimer, which is like two or three chains wound around each other. In this case, the heterodimer has several chains twisted together, a vitamin D component, a vitamin A component, and a vitamin K2 component.
The osteoblast cannot fire into action without its DNA being stimulated by this twisted up chain of vitamins. Also twisted into this chain is thyroid, in the form of T3 (triiodothyronine). The DNA then gears up the cell to start making a gooey ooze called osteocalcin. In this ooze, the calcium is bound up and solidifies the bone structure.
To really speed up this osteogenesis, I prefer to add strontium which assimilates into the bone matrix much faster than calcium, AND it inhibits bone resorption as well which calcium does not. And calcium also can result in the production of stromelysin enzymes which cause cartilage resorption, potentially worsening osteoarthritis. There are many studies that show the efficacy of different forms of strontium in osteogenesis. One study out of Canada used micronutrient therapy with a combination of vitamin D3, vitamin K2, strontium, magnesium and docosahexaenoic acid (DHA) with good results (COMB protocol: Genius and Bouchard, Journal of Environmental and Public Health Volume 2012).
I also recommend the addition of vitamin A and if levels are low, thyroid hormone.
Please appreciate the contrast between SLOWING BONE RESORPTION and STIMULATING BONE FORMATION.
I also add glucosamine and chondroitin to this combination of micronutrients because there are studies that indicate strontium and these two supplements may enhance cartilage formation in the joints and prevent cartilage resorption and may therefore be “disease modifying osteoarthritis drugs” (DMOADs) (Jerosch, International Journal of Rheumatology Volume 2011; Rodrigues et.al., Brazilian Journal of Medical and Biological Research (2018) 51(8); Reginster, et. Al. Ann Rheum Dis 2013;72:179–186).
Based on the science, this is an intriguing possibility.
So much for monotherapy in osteoporosis!