Introduction
Before I get into my protocol, let me tell you a story. Last week I admitted a patient to the rehabilitation hospital who had been seen at one of the local hospitals in the medical center in Houston. She is typical of the stroke patients that I see several times a week. She is a youthful 70 year old woman who had been living alone independently in Galveston, driving and participating in community activities.
She was spending the Christmas holidays with her daughter in Houston when she suddenly had a paralysis in her left arm. This slowly resolved over the space of several hours, and she insisted to her daughter that she was fine. However, this paralysis recurred several hours later. Her daughter, realizing something was indeed wrong, took her to the emergency room where the routine CT scan of her brain and an EKG were performed, both of which were normal. This is usually the case with strokes because, if there is no bleeding in the brain, the CT will be “negative” for the first 2 or 3 days after a stroke. After this time, the CT will show the areas of dead and ischemic brain tissue. The EKG is performed to rule out an arrhythmia of the heart that could have set up intracardiac clots that could have dislodged and been pumped up to the brain. Since both of these were negative and since the paralysis had again resolved, she was told she had not had a stroke and to go home and make an appointment with a neurologist.
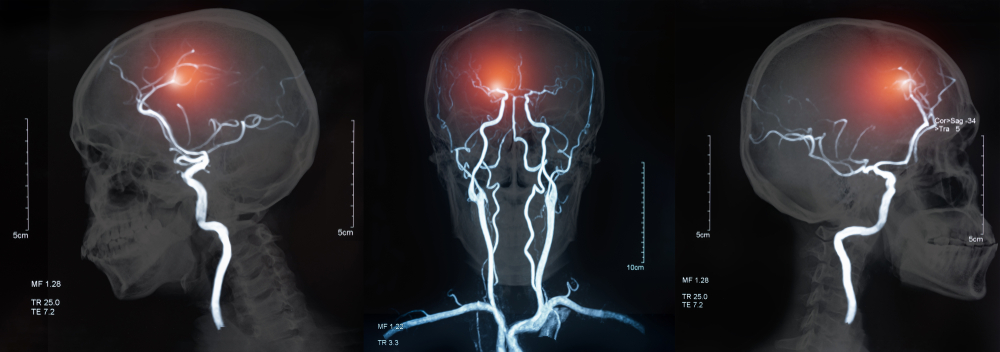
When she finally saw the neurologist, she was told that, in fact, she had indeed had a stroke and was sent for Doppler scans of her carotid arteries which showed a 95% stenosis or narrowing of the right carotid artery. However, before she received the report of these results, her left arm paralysis recurred, and this time it did not resolve. At this point she was finally admitted to the hospital with the diagnosis of a stroke.
The unfortunate truth here is that this woman was having an evolving or stuttering stroke when she experienced her first episode of left arm weakness. The other unfortunate truth is that if doctors understood what happens at the cellular and neurochemical and biochemical levels during this early phase of the stroke, there is a good possibility that the whole event could be aborted before paralysis occurs. That’s what my protocol is about.
But let’s continue with our story. Once admitted to the hospital, a complete workup of her heart ensued. Echocardiograms and angiograms were performed at a cost of tens of thousands of dollars, all of which were also “negative”, and still NOTHING has been done to protect the brain cells that are still starving for oxygen.
The patient was then given aspirin and Aggrenox, which is the old “post-stroke formula” that we were all taught in medical school, but all these do is to slow down the aggregation or clumping together of blood platelets to prevent more clotting. She became nauseated on these medications when the doctors DOUBLED the dose, so it was changed to just aspirin and Plavix which is essentially the same medicine with less aspirin. In the meantime an MRI was performed of the brain that indeed showed, not one stroke, but multiple strokes involving both the occipital lobe (which accounted for her partial vision loss in her left eye of which she had also been complaining) and in the right frontal and parietal lobes of the brain (which accounted for her paralysis). These are the stroke areas of the brain that had been stuttering along for the several days prior to her admission to the hospital.
Since the patient had no cardiac problem and now that the stroke had been visualized by MRI and she had been started on her antiplatelet drugs, she had completed the “usual and customary” treatment for a new stroke. Nothing left to do now except to send her off to rehab and to tell the family and patient, “Yep, it looks like you’ve had a stroke.”
Yes, that’s all there is! That’s the medical treatment in 2009 for one of the most life-changing and debilitating events that can strike down a human being…and in America…..where we have the “best medicine in the world”. Our medical treatment of the stroke patient has not appreciably changed for the past 100 years except that in 2009 we can scan the brain with MRI and see exactly where the stroke is.
Think about this carefully. Much more is done for patients seen in the ER for a heart attack than for a ‘brain attack’. Large areas of heart muscle can sustain ischemic damage and the patient can still survive with all their motor, sensory, vision, speech, and cognition intact and they can return to a normal life. However, even a SMALL area of ischemic damage to the brain will ALWAYS have some functional deficit that profoundly affects a patient’s life.
It’s time to adopt a new emergent treatment plan for strokes that includes:
a. intervening in the chemical cascades that result in neuronal destruction occurring during the evolving ischemia; and
b. maximize local vasodilation to reperfuse this brain tissue; and
c. to bind receptors such as the NMDA receptors which will continue to propagate neuron death even after blood supply is restored; and
d. to reduce the free radicals released in enormous amounts during the stroke which continue to destroy more neurons and glia; and
e. to utilize biochemical mechanisms which minimize the damage resulting from the Ischemia-Reperfusion sequence.
These ongoing processes are the reason that the patient comes in initially with a weak arm and within 24 hours, the entire hemibody is paralysed.
I’ll show you how much more could have been done in an attempt to prevent the ultimate paralysis of this patient. All of these biochemical treatments I am suggesting are noninvasive and have been extensively published in hundreds of neuroscience and neurobiology journals, as I will also demonstrate.
So, if you’re reading this, you are wondering about strokes. Either you, one of your parents or other loved one has had a stroke and you want answers. You may be a doctor and, like me you have been struck with the revelation that in the past 50 years we have made virtually no advances in either the immediate management of stroke victims or any impact on diminishing the long term deficits which so profoundly affect the lives of these patients and their families. Your questions could and, in fact, should include:
“What causes a stroke?”
“What kinds of strokes are there?”
“How can I prevent a stroke?”
“What happens in the Emergency Room when a new stroke patient is admitted?”
“What should be done in the Emergency Room when a new stroke is admitted?”
“What can be done if I or my loved one has a stroke?”
“Is the damage permanent?”
“What can stroke rehabilitation do for a stroke patient?”
And for physicians, “What is the neuropharmacology of a stroke?”
These questions will be answered in great detail, perhaps even more detail than the layman might understand. However, in my attempt to change the current dogma and impotent management of this devastating process, I will need to delve into the current neuropharmacology research and this may be more science than the average person wishes to contemplate. As for the physician, our basic science training in medical school is a long time ago for most of us, but I feel certain that memories of these fundaments will quickly be refreshed in these doctors and they will unquestionably be able to understand the data and the merits of my protocols and the science on which it is based.
It is my sincere prayer that this will introduce a new protocol to the acute or emergent management of the stroke patient. It is also my hope that the research presented which is published in highly reputed journals and reviewed prior to its original publication by some of the world’s foremost scientists will be appreciated for its scientific merit and the layman and physician alike will see the potential for its practical application in the care of the stroke patient.
In addition, I would like to see, utilizing information and concepts presented in this book, well-designed scientific studies of biochemical, structural, and functional outcomes in stroke patients. Perhaps we can impact stroke outcomes by implementing these basic biochemical and neuropharmacologic interventions and bring about a long overdue change in the management of stroke, brain injury, and spinal cord injury
An Overview
It is important to understand the physiologic and biochemical rationale for this protocol and to this end I will divide it into two basic parts. First, I will describe the mechanisms of neuron damage and death and then discuss the neurochemical interventions that will obviate this cascade. Second, I will present the evidence for neurogenesis which is the process by which stem cells in the brain and spinal cord can be stimulated to differentiate into nascent neurons and mature to become functional brain and spinal cord cells.
Phase 1: Ischemia
The most common injury to the nervous system is a stroke. In the first phase of a stroke, there is a blockage or occlusion of an artery that feeds a part of the brain. This is called ischemia. This robs the neurons in that part of the brain of its vital oxygen and glucose which are essential to the brain cell survival. If the blood flow is not quickly restored, these neurons will die, just like myocardial cells in a heart attack. Unfortunately, unlike heart muscle, brain cells cannot tolerate ischemia for long. In a heart attack, doctors can restore the blood flow with medications and with angioplasty. However, in the brain we have neither the time nor the ability to get access into the brain arteries to reopen them with angioplasty. We can, however, use drugs and chemicals to dilate these arteries and reestablish blood flow to the brain. So what drugs should we use?
First, we need to understand the sequence of the biochemical events that occurs in ischemia in order to know what medications might be useful to counter these events and restore oxygen and glucose to these brain cells.
Initially after the artery plugs up, the body tries to make nitric oxide (NO) to dilate it as well as other arteries that might feed the same brain tissue. It uses an amino acid arginine which is acted upon by the enzyme nitric oxide synthetase (NOS) to produce NO. If there is inadequate arginine available, this chemical reaction cannot occur and the vessels remain constricted and the neurons continue to starve for oxygen and glucose. However, if there is adequate arginine, nitric oxide synthetase can utilize it to make nitric oxide and increase blood flow to the ischemic cells.
The endothelium will also try to make NO from Estradiol and from Insulin Growth Factor 1 (IGF1) which is produced from Human Growth Hormone (HGH). Again, if these hormones or substrates are not in adequate supply, the production of NO will be compromised and vasodilatation cannot occur.
Phase 2: Oxidation
The second phase of ischemic brain injury is the direct result of cell death. It involves the production and release of oxidants or free radicals and when these are spread through adjacent tissue, more neurons die. The “Ischemia-Reperfusion” sequence produces many species of highly destructive free radicals and is extensively discussed in the cardiovascular literature as it relates to myocardial infarction and cardiac bypass grafting. It is very well known that reducing membrane oxidative potentials by pretreating patients undergoing bypass grafting with various antioxidants will minimize any tissue damage resulting from the ischemia-reperfusion process.
In the brain, one of the most destructive of these free radicals released in ischemia is peroxylnitrite which will be discussed in more detail in later sections. This chemical when released will kill more neurons by free radical action on cell membranes and the mitochondria, as well as glial cells which support neurons and produce myelin to insulate the axons.
Phase 3: Inflammation
The inflammation phase of stroke is the next phase of the cascade of events and is mediated by a number of factors in addition to the free radicals mentioned above. The free radicals cause the production and release of inflammatory cytokines. Independent of cytokine release caused by the free radical production, the body produces even more of these cytokines as a result of the ongoing ischemic injury. Cytokines increase the inflammation which produces even more cytokines. In addition to this cytokine release, there is also a release of matrix metalloproteinases which are potent inflammatory agents resulting in even more local cytokine destruction of neuronal tissue and more platelet activation which can in turn occlude more blood vessels, thereby expanding the size if the stroke.
Phase 4: Release of Excitotoxic Neurotransmitters
Aspartate and Glutamate are excitatory neurotransmitters that occur normally throughout the brain and function just like other neurotransmitters such as norepinephrine, GABA, serotonin, etc. They are not toxic as long as they remain in their own respective neurons and the receptors intended to receive them. However, if they are released into the tissues and contact other neurons not intended to receive them, they are highly toxic to these cells.
SUMMARY:
So this is why a stroke patient comes into the ER with a slight weakness in one arm and 24 hours later, the entire right or left side is paralysed. It is a cascade of events which evolves over a period of time beginning with a small arteriole occlusion but ending with a large area of destroyed neurons.